August 2022
Much of the discourse that surrounds Frantz Fanon has historically focused heavily on his writings on political violence and revolutionary action in the colonial and postcolonial context, failing to connect this writing to his work as a psychiatrist during the Algerian War of Independence. Although Fanon remains a figure of revolutionary writing and action, he also made significant contributions to scientific and medical discourse and practice. Acknowledging these aspects of Fanon’s work not only highlights previously untouched parts of Fanon’s life, but also provides an important lens into the continuities between his psychiatric and political work, and to the continuities between psychiatry and political economy in general. Some recent scholarship has highlighted these crucial connections. In Frantz Fanon, Psychiatry and Politics, for example, Nigel C. Gibson and Roberto Beneduce ask whether it is “possible to make free associations in a dispossessed world.”[1] Referencing Freud’s talking cure, they bring attention to the challenges that social, political, and colonial specificity bring to any project of standardized psychopathology. The authors place Frantz Fanon’s clinical psychiatric work, some of which is translated from the French for the first time, into the scholarship that surrounds the psychiatrist and political theorist’s legacy. Fanon’s work makes it clear that psychiatry and politics are fundamentally inseparable, and his psychiatric and political legacies should be likewise. Here I hope to demonstrate the importance of connecting the two, often using Gibson and Beneduce’s newly-translated sources to interrogate the social-neurological divide in psychiatric discourse.
Overcoming the Social-Neurological Divide
Within Fanon’s critique of colonial psychiatry lie implicit and crucial insights into contemporary debates about psychiatric reductionism. Historically, paradigms in psychiatry have shifted between explanatory modes that focus on purely biological causes of psychopathology and modes that focus on more social-psychological or at least interpretative ones.[2] While biological reductionist methods seek to identify the cause of psychiatric illness through individual biological markers, such as a neural pathway or a gene, psychological explanations acknowledge a philosophical or interpretative aspect to the subjective experience of psychiatric illness.
In the past few decades psychiatric reductionism has fallen out of fashion, following the ambitious Human Genome Project (HGP) in the 1990s (the period that George W. Bush named “The Decade of the Brain”). Many critics not only identified potential injustices and links to eugenic thinking in these projects, but also noted their ultimate inability to convincingly reduce mental experiences to physical markers in the body. In Psychiatric Hegemony, for example, Bruce Cohen sketches a Marxist theory of mental illness and psychiatric treatment which critiques the way that the biomedical approach to psychiatric illness “conceptualizes disease as a physical pathology of the body… that can be observed, measured, and treated.”[3] At the end of the day, Cohen points out, the claim that mental pathology is strictly biological simply “lacks the legitimacy of scientific evidence.”[4] The ultimately inconclusive results of projects like the HGP support his claim. The pendulum often swings too far in the other direction, however: although Cohen provides important insight into the sometimes faulty logic of biomedicine, his historicist method runs the risk of collapsing the subjective dimensions of “mental illness” into purely political terms, falling upon a straightforward narrative of medicalization. When the “social construct” model of mental illness is pushed to its logical extreme, it can result in a form of social reductionism, rather than providing a critical but robust theory of psychiatry and legitimate psychical suffering.[5]
In contrast, Frantz Fanon’s psychiatric work engaged with the biological, the social, and the psychological[6] in a way that acknowledges the complicated interconnectedness of all of these aspects of mental illness. Fanon argued that mental illness exists in the intersection between (always political) subjectivity, individual biology, and relations of social production; it is not so constructed as to not have a material basis in reality. His doctoral dissertation dealt with the tensions between neurology and psychiatry, highlighting the “autonomy of psychic disorder even in a hereditary neurological disease, [and] the role of social context in determining different [biological] expressions of personality.”[7] Here, Fanon was explicitly interested in the way that the social had direct effects on biology, rather than throwing the category of biology out altogether: a more radical understanding of the way that capitalist and colonial relations affect the body directly. In this way, Fanon preempted the many discussions of the ways that poverty and racism affect the body and physical health today such as the popularly-cited Adverse Childhood Experiences study or Basel A. van der Kolk’s The Body Keeps the Score. What these two contemporary texts lack, however, is the radicality of Fanon’s arguments about what one should do with the idea that colonialism quite literally imprints itself on the body on a cellular level.
While the Adverse Childhood Experiences study encourages working within the (broken) social welfare system to heal individuals, and van der Kolk encourages somatic self-healing stripped of much collective engagement, Fanon argued that we cannot ever hope to heal the individual without collective revolutionary transformation, and vice versa. Gibson and Beneduce’s book eloquently illustrates how Fanon’s engagement with both Marxist and psychoanalytic schools of thought shaped this unique perspective on the multidimensionality of psychiatry. It is Fanon’s combination of psychoanalytic and anticolonial Marxist thought that allows him to explore how we might adequately treat both psychiatric illness and sociopolitical injustices that are inseparable from the lives of psychiatric patients and doctors alike. We cannot expect to treat individual suffering without seeing the breakdown of colonial power; likewise, we cannot expect to engage in true anticolonial action without a commitment to understanding the ways that colonial relations lodge themselves into the unconscious—an unconscious that includes the physical body.
Hysterical Paralysis and Colonial Violence
What follows is an attempt to highlight the timeliness of revisiting Fanon’s work by putting it into context with the work of Edward Shorter, a historian of psychiatry. I hope that this will demonstrate some of the ways that psychiatric symptoms have evolved over time and provide compelling evidence for some of Fanon’s arguments. It is important to trace the connections between the biological and social facets of psychiatric illness. Shorter has already done this with the phenomenon of hysterical paralysis in his article, “Paralysis: The Rise and Fall of a ‘Hysterical’ Symptom”. [8] Hysterical paralysis was an epidemic in the late nineteenth century industrialized world—people, often women, presented with paralysis of their limbs, the inability to speak, incontinence, and seizures among various other neurological symptoms with no identifiable biological cause. The term evokes Charcot’s photographs from the famous Salpêtrière hospital:
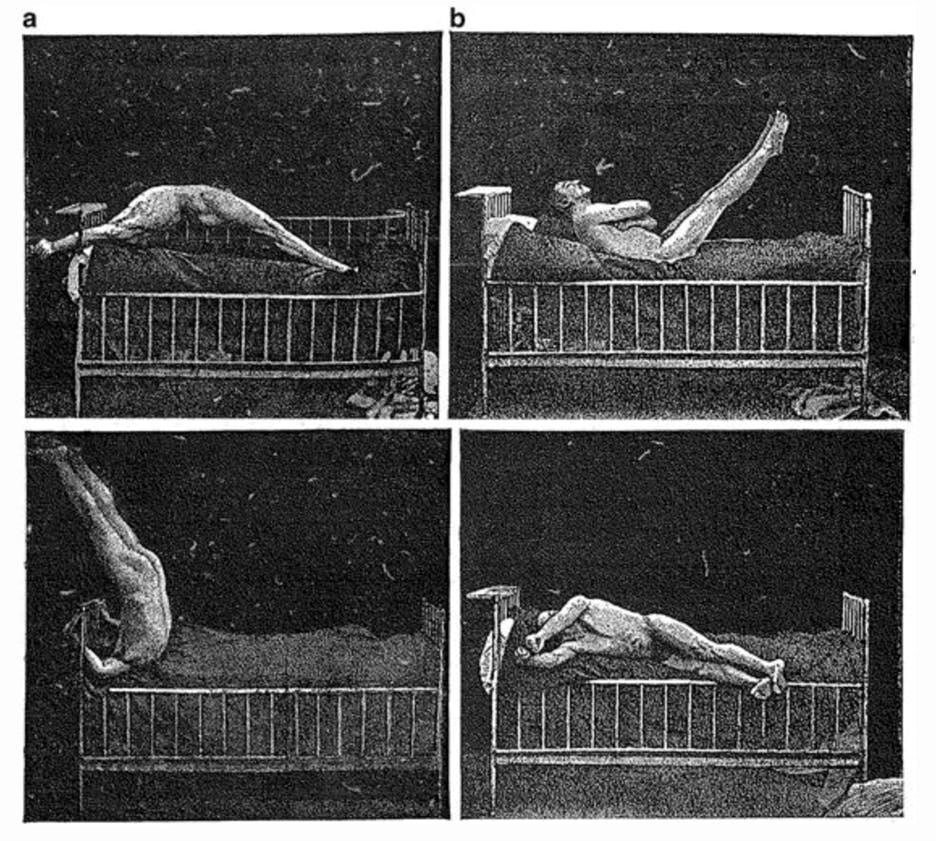
Hysterical paralysis is a paradigm of psychosomatic disorder: the body fails to function, refuses to move, with no injury or degenerative pathology to explain this failure. Although hysterical paralysis proliferated after periods of high industrialization, it eventually waned and is now considered a rare conversion disorder, almost a vestige of the past. Unlike viral epidemics, however, there is no disease entity with which we might trace the evolution of this epidemic and eventual adaptation of our species to its influence. How might we understand the rise and fall of a psychosomatic phenomenon, then?
Shorter employs a method unexpectedly similar to Fanon’s social-psychological-biological theory of mental disease in order to explain the occurrence and eventual disappearance of hysterical paralysis. Throughout the article, Shorter provides social and historical context for hysterical paralysis, adding a much-needed social dimension to the historical diagnosis. However, he does not explain away the diagnostic category of hysteria by claiming it is entirely a misogynistic construction used to control women or pathologize their behaviors. After all, the disorder did exist, it did result in significant disability, and it did occur primarily (at least in the historical record) in women. Shorter argues that it is clear that hysteria “is a real psychiatric disease” because it physically presented itself in huge populations of women and lower-class male patients, “in addition to being an epithet with which men have stigmatized women across the ages.”[9] The stigmatization came afterward, in what seems like an inevitable precipitate of any affliction primarily experienced by women in a patriarchal society. Shorter continues to highlight the material reality of hysterical paralysis despite its complicated social life: “Even after we have stripped away the cultural layers of male hostility and medical uneasiness in the face of female sexuality which the diagnosis has often conveyed, we still confront a group of predominantly female patients who are unable to walk, to get out of bed, or relax their contracted ankle muscles.”[10]
So why did these very real paralyses happen, despite their imbrication in patriarchal power? The complicated question that Shorter poses here is how we can understand a psychiatric illness as a social phenomenon without dismissing the disease category altogether. This is as much a historiographical question as a social one: how can we understand hysterical paralysis at once as a subjective experience and as a biological phenomenon directly influenced by social norms (in this case, patriarchal norms)? More broadly, how does the social or the political materially inscribe itself in the body, in this case via psychiatric illness?
The main model that Shorter uses to understand hysterical paralysis is what he calls the “symptom repertoire;” the “range of physical symptoms available to the unconscious for the physical expression of psychological conflict” in psychiatric patients.[11] The symptom repertoire can be defined as the set of available pathological concepts in any culture that people have internalized, which can present as functional symptoms[12] in the absence of a straightforward physical etiology, or cause. This is precisely where Fanon’s work is useful, in that Fanon was as much concerned with the symptoms of individual psychiatric patients as he was with the symptoms of colonial society as a whole; more importantly, he was concerned with how the microcosm of the individual patient is always in a dialectical relationship with the macrocosm of colonial society. In order to cure psychiatric illness, Fanon maintained, we cannot simply address the individual; rather, we must also chip away at the structure of colonial society to relieve the very real psychiatric illnesses that are part and parcel of its existence. If we want to understand hysterical paralysis, we have to understand why huge numbers of women experienced it in its historical specificity (here, post-industrial capitalism). And if we want to cure it, we can’t expect the bodies of these women to fix themselves independently of the society that encouraged the symptom. This is not to say that all mental suffering will wither away with the colonial state. Gibson and Beneduce argue that “while Fanon believed that organized political action was essential to individual and social liberation, he was under no illusion that it exhausted the problem of mental illness and suffering.”[13] Fanon’s interest was rather in identifying and always maintaining awareness of how the sociopolitical informs the psychological so as never to lose track of the project of building a better society both in totality and for each individual within that totality.
As Gibson and Beneduce point out, one of the defining features of Fanon’s work is his ability to shift “between politics and psychiatry, between the social and the subjective, between the unconscious and history.”[14] Although many simplistic interpretations of Fanon argue that he believed psychiatric ills and trauma will be cured in a post-revolutionary society, Fanon was in fact interested in the relationship between the psychiatric and the political—in the ways that both categories inform and construct one another, never in a unidirectional manner but always in dialectical relationship to each other. The effects of colonialism and capitalism on the body will not simply disappear after the social order changes: that takes dedicated work and healing with individuals and collectives even when their social, political, and economic conditions improve. By attempting to understand this complicated relationship, Fanon was able to elucidate some of the ways that psychiatric illness in colonized subjects can in fact reveal contradictions in colonial society that work to oppress these individuals. As Gibson and Beneduce argue, if “we accept that symptoms speak, as Lacan and Freud [argued], and that the colonized reveal in their suffering a specific form of historical consciousness, Fanon must be acknowledged as a pioneer of critical ethnopsychiatry.”[15] Psychiatric symptoms, according to Fanon, might give us insight into the specific ways that colonial violence lodges itself intimately into the bodies and minds of its subjects.
Fanon and Critical Ethnopsychiatry
Fanon’s engagement with the mind-body effects of colonialism began with his doctoral dissertation, which was situated firmly within the discourse of scientific psychiatry. He began his medical degree at the University of Lyon in 1946. His doctoral thesis was at first primarily about the importance of social influences on psychopathology and its treatment, but it was rejected by his department, which was predominantly organicist at the time. In order to appease the department’s demands to focus on the biological dimensions of psychiatric illness, he added a study on Friedreich’s Ataxia (a neurophysiological disorder) and delusions of possession, and this version of his thesis finally met his supervisor’s approval.[16] Although Fanon was able to make his work conform to the demands of his department, his “methodological perspective, and his placing of the symptoms of mental disorders in their social and historical contexts, was without a doubt troubling for the science of mental health at the time.”[17] His methodology, even in this very early work, concerned the dialectical relationship between thinking and being, between the organic and psychical, and between neurology and psychiatry. He grounded this methodology in the work of Henri Ey, a French neurologist, Kurt Goldstein, a German neurologist and physician, and Jacques Lacan, the French psychoanalyst.
Fanon’s doctoral dissertation insisted on giving symbolic meaning to the content of delusions, even in the presence of an organic brain disease. While organic neurophysiological diseases were often treated as if the subsequent delusions had no meaning and therefore no relevance in treatment, Fanon argued that “it is necessary to consider patients’ mystical beliefs not simply as an expression of their ‘intellectual insufficiency’ [via organic brain disease] but in terms of a complex reaction—‘a biological, psychic, and metaphysical restriction’—to the inexplicable.”[18] Fanon was able to provide a more robust explanation of organic brain disease and accompanying delusions using these methods. Ultimately, this early scientific work would foreground Fanon’s later clinical work and continued commitment to understanding psychiatric symptoms as phenomena that are inextricably embedded in history and language and therefore in historical consciousness.[19]
In their book, Gibson and Beneduce introduce another less-acknowledged facet of Fanon’s work: his development of what they call a “critical ethnopsychiatry.” John Colin Carothers, a contemporary of Fanon’s, developed the tradition of ethnopsychiatry in the early 20th century as a method to understand psychiatric illness in Africa. Unsurprisingly, Carothers and his colleagues based their ethnopsychiatry on biological racism, as their goal was to “produce a portrait of the ‘African mind,’ showing how this differs from the European ‘norm’ interpreting African personality and behavior predominantly in the form of symptoms.”[20] Carothers was supported financially and ideologically by the World Health Organization. Fanon’s proximity to Carothers and his colleagues encouraged Fanon to ask further questions about the injustices in psychiatry he saw legitimated by a biological model of not only psychopathology, but also race—in this case, the two were inextricable for Carothers’s scientifically racist psychiatry.
It is in Fanon’s relationship to racist ethnopsychiatry that we can understand another unique contribution of Fanon’s to the biopsychosocial model of mental illness. As Fanon developed his critical ethnopsychiatry, the explanatory element that would make Fanon’s work so robust was his inclusion of structural causes in the symptomatology of colonized psychiatric subjects. This work was developed while Fanon worked at the Blida-Joinville Hospital in Algeria in 1953, right before the Algerian Revolution. While working at Blida-Joinville, Fanon published some scientific articles with his colleague Slimane Asselah regarding their clinical work in the clinics, including “The Phenomenon of Agitation in Psychiatry,” where Fanon and Asselah traced the “political semiotics” of agitation in their patients.[21] By engaging with political semiotics, Fanon and Asselah were trying to understand the structural forces beneath the formation of seemingly neurological/biological psychiatric symptoms. They critiqued their mentor, François Tosquelles, who proposed that there are two types of agitation: one, percepto-reactive or “dominated by a mechanism of perception and reaction,” and the second, “primarily expressive.”[22] Fanon and Asselah, in contrast, argued that agitation is not a “mere symptom” but also a reasonable response to the structural issues in colonial psychiatry: they argued that “the fact is that the hospital itself is sadistic, repressive, rigid, nonsocialized, and castrating.”[23] Agitation was not a “mere symptom,” then, as it was also a social relation between hospital staff and their patients: “Fanon and Asselah insisted that all forms of agitation are products of reciprocity; that is, they are triggered and sustained by human relationships.”[24]
What is unique here is Fanon and Asselah’s use of the structure of society to directly explain the presentation of symptoms in patients. The occurrence of agitation in patients was not due to singular, isolated instances of repression between staff and patients; rather, it was written into the structure of the colonial hospital itself. This complicates the very idea of “pathological” behavior in the colonial context: it is here that “diagnostic categories lose their clinical value and simply mirror institutional violence.”[25] Additionally, this analysis allowed Fanon and Asselah to understand how places of healing (psychiatric hospitals) had become “paradoxically … a cause of further suffering.”[26] While Tosquelles had made headway by arguing that agitation was always subjective and individual, Fanon and Asselah were able to expand this subjective reductionism into a map of structural colonial violence that was inextricable from psychiatric institutions like Blida-Joinville: in this case, the political semiotics of psychiatry helped to make Fanon’s engagement with biology, the social, and the psychological and their interrelationships more robust. This is one example of the continuities, rather than differences, between Fanon’s psychiatric and political work. In fact, Fanon’s political awareness of colonial violence began to develop as a direct result of his psychiatric work at Blida-Joinville. Although Fanon was still invested in understanding why certain symptoms presented in African subjects, engaging in ethnopsychiatry, he was critical of the idea that these symptoms were essential to the African subject. Instead, they grew from social, racial, colonial relations.
Fanon’s development of critical ethnopsychiatry is complementary to Shorter’s work. In 1954, Fanon continued to publish psychiatric articles now with his colleague Jacques Azoulay, resulting in (per Gibson and Beneduce) “critical reflections” that “threw off any remnants of the psychiatry of the Algiers School [of Carothers], and set the psychical suffering of many of the patients within the flux of historical events and the net of symbols that contained their existence.”[27] This “net of symbols” that encompassed psychiatric symptoms resonates with Shorter’s concept of the symptom repertoire. For Fanon, the net of symbols was precisely what influenced his patients’ presentation of psychiatric symptoms, much like Shorter’s symptom repertoire provided the set of available symptoms for women with hysterical paralysis. However, while Shorter’s analysis ends by arguing that “something about the logic of capitalism may have been acting in historically unprecedented ways to produce these paralyses,” Fanon provides a deeper critique of not only capitalism but also colonial domination.[28] Additionally, the structural element of Fanon’s work adds to the idea of the symptom repertoire by providing a method for understanding psychiatric symptoms as collective cultural experiences. While it is useful to understand individual symptoms as part of a reaction to that individual’s social world, Fanon’s structural analysis adds a way to conceptualize collective action in relation to colonial psychiatric symptoms. In other words, patients never experience this subjugation or these symptoms alone: they maneuver through structures that require resistance through collective action. In this way, then, collective political consciousness can only be achieved if we acknowledge psychiatric symptoms in populations of colonial subjects.
Fanon's Interventions as Revolutionary Practice
Fanon’s clinical practice in colonial psychiatric hospitals led directly to his revolutionary political work. Contrary to some narratives, Fanon was not driven to some divergent revolutionary cause in contradiction to his psychiatric practice. Rather, Fanon was forced to confront a problem of consciousness in colonial society itself. While many European psychiatrists attempted to understand pathology in a rationally scientific manner specific to the colonial center and never the peripheries, Fanon noticed that pathology in colonial hospitals doesn’t function “rationally,” at least not in a way correlated to European standards of rational behavior. If Shorter’s symptom repertoire has the advantage of bringing historical specificity to psychiatric symptoms, Fanon’s clinical work adds a crucial dimension of colonial specificity. Furthermore, it was precisely the identification of these colonial contradictions that led Fanon to leave his clinical work to engage in revolutionary work during the Algerian War. For Fanon, it became clear that an ethical psychiatry could not exist in a world that continued to operate under colonial structures; therefore, he began to work to dismantle these structures. He could not have come to these conclusions at all had it not been for his clinical psychiatric work. Fanon’s decision to join the FLN was intimately tied to his commitment to understanding psychopathology, not a turn away from medicine.
Gibson and Beneduce are able to solidify this historiographical argument by ending with Fanon’s later work, including Wretched of the Earth. In this book, published in 1961, they argue that “the more Fanon the political revolutionary advanced in imagining the new society, the more Fanon the psychiatrist could not forget the wounded society on which the new nation would be built.”[29] Here Fanon returned not clinically but conceptually to psychiatry and theories of psychopathology. Fanon could not forget how political violence materially embedded itself in the consciousness of colonial subjects: “an entire generation of Algerians,” he argued in Wretched of the Earth, “steeped in collective, gratuitous homicide with all the psychosomatic consequences this entails, would be France’s human legacy in Algeria.”[30] Gibson and Beneduce end their book by highlighting the often cyclical nature of racial stereotypes regarding violence. They argue that it “is amazing … there has been such insistence on reading the first chapter of The Wretched of the Earth (titled ‘On Violence’) as an apology for violence, and that so much time has been dedicated to discussing Fanon’s theory of violence” when “what has been overlooked is [Fanon’s] desperate analysis of the violence that the colonized are condemned to act out and repeat.”[31] In other words, the violence that Fanon engages with is directly connected with what colonial society does to its subjects: there is nothing essential about this violence to the people of Algeria, for example. Racial stereotypes about violence, and now even psychiatric stereotypes, are denaturalized and put into the context of political economy and the effects of colonization on its subjects. Fanon’s work at Blida-Joinville gave him crucial insights into what colonialism does to the body and minds of the colonized. We cannot separate these observations from Fanon’s calls to action and revolutionary violence. Beneduce and Gibson ultimately show us that Fanon’s psychiatric work gave him a unique lens into the pathology of colonial society itself, including the long and arduous process of developing a new society in a potentially post-colonial world. Fanon knew that even after the liberation of colonized subjects, traumatic memories would not simply disappear, either individually or collectively, and he dedicated his life to trying to understand how to heal before, during, and after revolutionary action.
Notes
1. Nigel C. Gibson and Roberto Beneduce, Frantz Fanon, Psychiatry and Politics (London: Rowman & Littlefield, 2017), p. 157.
2. Hannah Decker, for example, identifies psychiatry’s tendency to historically “[swing] between emphasizing material (somatic) paths and non-material (psychological/experimental) avenues to knowledge.” Decker argues that in the last two centuries, psychiatric research and knowledge production have oscillated between favoring either interpretative, theoretical, psychological explanations of mental disorders, or medical, material explanations of mental disease. See Hannah Decker, The Making of DSM-III: A Diagnostic Manual’s Conquest of AmericanPsychiatry (Oxford: Oxford University Press, 2013). Quoted here is p. xix.
3. Cohen, Psychiatric Hegemony, 5.
4. Ibid.
5. Although it is tempting to attribute most, if not all, forms of mental illness to structural issues, I believe that this form of social reductionism further strips agency away from those who are suffering. A substantial amount of empowerment results from acknowledging that your psychiatric conditions are partly due to generations of oppression and the inability of capitalism, imperialism, and/or heteropatriarchy to accommodate us. However, stopping at an external critique often only suspends us in another state of arrested development, in that personal agency and responsibility towards the self and others is never encouraged in many of these constructionist models of mental illness. Recognizing the conflicts in one’s relationship to others in the context of systemic oppression is important, and being angry with what caused these conflicts is an important step in resolving them. In the tradition of Marx, however, “the point is to change it.”
6. While many contemporary models of psychiatry see “biopsychosocial” models as the most useful way to understand mental illness, they tend to hierarchize the three, where the biological has the most explanatory power and the social has the least. In contrast, Fanon uses the social as a point of causal reference as opposed to just one explanatory factor so as to rearrange the whole epistemology of biomedical psychiatry itself.
7. Gibson and Beneduce, 38.
8. Edward Shorter, “Paralysis: The Rise and Fall of a ‘Hysterical’ Symptom.” Journal of Social History 19, no. 4 (1986): 549-582.
9. Ibid, 574.
10. Ibid.
11. Ibid, 549.
12. A functional symptom can be understood as what we call a “psychosomatic” symptom today, although it has more historical specificity. In the late 19th and early 20th centuries, European neurological psychiatry was concerned with finding the localized origin of neurological symptoms: for example, seizures could be sometimes traced to lesions in the brain. A functional symptom, however, was a symptom that could not be traced back and localized in any organic lesion in the brain itself. Often, these symptoms were explained psychologically as a result of the lack of a physical cause (much like today’s psychosomatic symptoms). However, it should be emphasized that just because a symptom is functional, it does not mean it isn’t physical. In some contemporary discourse surrounding psychosomatic illness, psychosomatic symptoms are treated less “real” because they come from the patient’s “mind” as if to imply it’s “all in their head.” However, psychiatrists have long tried to understand symptoms scientifically as physiological ailments so as not to dismiss patients’ concerns as fabricated and less “real.”
13. Gibson and Beneduce, 5.
14. Ibid, 2.
15. Ibid, 22.
16. Ibid, 37.
17. Ibid, 40.
18. Ibid.
19. Fanon’s work with language and meaning is discussed in more detail in Chapter 1. The authors quote Patrick Ehlen (2000) describing Fanon’s psychiatric methodology at length: “The task of the psychiatrist, then, becomes not simply to interview the patient and then thumb through a book to uncover the diagnosis and solution, but to make an effort to ‘reach’ the patient through the patient’s own symbols and belief system … or even beyond the patient, as the psychiatrist struggles to uncover those cultural ‘participations’ at work in the patient’s psyche” (Ehlen 2000: 99). The delusions present even in organic illness, therefore, would grant a psychiatrist access into not only the meaningfulness of their own symptoms, but also to the symptomatic structure of colonial society that directly informs the construction of symptoms to begin with.
20. Gibson and Beneduce, 102.
21. Ibid, 139.
22. Ibid.
23. Ibid, 140.
24. Ibid.
25. Ibid.
26. Ibid.
27. Ibid, 159.
28. Shorter, 573.
29. Gibson and Beneduce, 232.
30. quoted in Gibson and Beneduce, 233.
31. Ibid, 254.
